Surgical Retina
At Wollongong Eye Specialists, we can offer our patients expertise, and the surgical management of the following conditions and diseases affecting the retina, the light-sensitive tissue at the back of the eye.
Each of these conditions and their possible treatment and surgical strategies are detailed on this page.
Please do not hesitate to reach out to us if you would like more information, seek a consultation, or would like to organise a referral to our care for any of these ophthalmic issues.
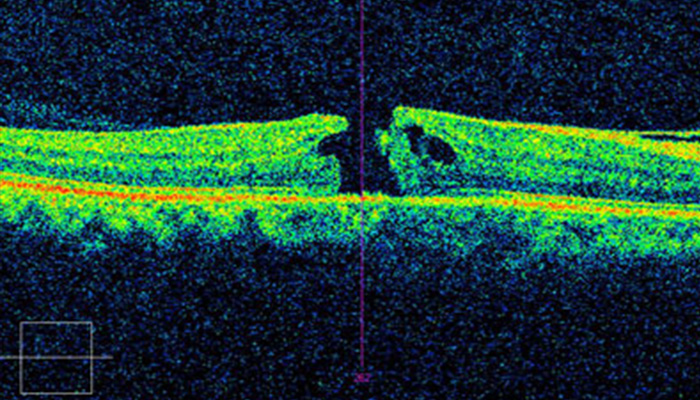
Macular Hole
A macular hole is a small break or tear in the macula, the central part of the retina responsible for sharp, detailed vision used for activities like reading, driving, and recognising faces and any damage to it can significantly impair visual clarity.
Age related and more common in people over 60, a macular hole typically occurs due to changes in the vitreous, the gel-like substance inside the eye. As we age, the vitreous can shrink and pull away from the retina, sometimes causing a tear or hole in the macula.
The key causes can include:
- Age – most macular holes are age-related due to the natural shrinkage of the vitreous, this is also called posterior vitreous detachment.
- Trauma and injuries to the eye can cause macular holes
- Diabetic retinopathy can lead to the formation of macular holes
- Macular holes can also occur in association with retinal detachment, macular pucker (wrinkling of the retina), or high myopia (near-sightedness).
Symptoms of a macular hole can include:
- Blurred central vision: People with a macular hole may notice a blurring or distortion of their central vision however peripheral vision is typically unaffected.
- Distorted vision: Straight lines may appear bent or wavy.
- A dark or empty spot in the central vision: This is especially noticeable when trying to read or focus on objects.
Treatment
Treatment of macular holes can include the below and your eye doctor will discuss with you the most appropriate for your individual eye heath.
- Observation and monitoring as with some cases a macular hole can close on its own without intervention.
- Vitrectomy is the most common surgical treatment for a macular hole. The procedure involves removing the vitreous gel and replacing it with a gas bubble. The gas bubble helps press the edges of the hole together, allowing it to heal. Over time, the eye absorbs the bubble, and the vitreous space fills with natural fluids. Patients usually need to remain in a face-down position for several days after surgery to help the bubble press against the hole.
If untreated, macular holes can lead to permanent central vision loss. Early diagnosis and treatment improve the chances of successful recovery of vision.
Epiretinal Membrane (ERM)
Epiretinal membrane (ERM) is a thin, transparent layer of fibrous tissue that can form on the surface of the retina, specifically over the macula, and can cause visual distortion and blurring, especially when it contracts or wrinkles the macula.
ERM’s are generally not dangerous but can cause discomfort and vision issues that affect quality of life and depending on severity and the patient’s visual goals monitoring and treatment is recommended.
The causes of ERM are detailed below.
- ERM is often age-related and can occur because of natural changes in the vitreous gel within the eye. As the vitreous shrinks, it can pull away from the retina, stimulating the formation of scar-like tissue on the macula.
- Posterior vitreous detachment (PVD) is a common cause of ERM, as it can lead to damage to the retina, triggering the ERM formation.
- Retinal tears or retinal detachment can stimulate the development of ERM.
- Eye trauma or surgery such as cataract surgery or a sudden impact, can lead to the formation of an ERM.
- Inflammation inside the eye, such as uveitis, can also contribute to ERM formation.
Common symptoms of ERM include:
- Blurred or distorted vision: Straight lines may appear wavy or bent and central vision can become blurry and some may experience double vision in the affected eye.
- Difficulty reading or seeing fine details, especially in more advanced cases.
- Loss of central vision: In severe cases, ERM can lead to a significant decrease in central vision, though it typically progresses slowly and does not cause complete blindness.
Treatment
Treatment of ERM can include the below and your eye doctor will discuss with you the most appropriate course of action for your individual eye heath.
- Observation: In mild cases where vision is only slightly affected, treatment may not be necessary, and the ophthalmologist may work with you to monitor the condition over time.
- Vitrectomy: For more severe cases where vision is significantly impaired, surgical removal of the epiretinal membrane may be recommended. This procedure involves a vitrectomy, where the vitreous gel is removed, and the membrane is carefully peeled off the macula to relieve the distortion. Vision often improves after surgery, but complete recovery may take several months, and full visual acuity may not always return.
Retinal Detachment
Retinal detachments are a potentially sight threatening condition that often requires urgent surgery or laser. The risk of getting a retinal detachment is about 1 in 10,000 but this risk is about five times greater for people who are short-sighted (myopic).
Symptoms that patients will describe noticing light flashes, or dark spots or floaters or a curtain like shadow coming across their vision.
It is imperative that you get your eyes assessed urgently if you believe you may have symptoms suggestive of a retinal detachment.
Treatment options for retinal detachment
There are several methods of surgery to treat retinal detachments, and your eye doctor will discuss the most appropriate option at your appointment. It is imperative that you get your eyes assessed urgently if you believe you may have symptoms suggestive of a retinal detachment.
Retinal detachment surgery is a day procedure, and you can recover in the comfort of your own home. Although you will be mobile, recovery should be managed over a 6-8 week period including time off work, avoiding driving and exercise limitations.
All of this, and your surgical options will be discussed with you at your consultation.
IOL Exchange
IOL exchange refers to a procedure in which an Intraocular Lens (IOL), previously implanted in the eye during cataract surgery or refractive lens exchange, is removed and replaced with a new one.
This procedure is performed when the initial IOL causes issues or does not provide the desired visual outcomes and is considered when other treatments, like glasses or contact lenses, are insufficient to address the visual problem. Your eye doctor will discuss possible options with you and recommend the best course of action depending on your current visual acuity and your visual goals.
The procedure is similar to cataract surgery and most often performed under local anaesthesia and the recovery process after an IOL exchange is typically similar to that of cataract surgery, with most patients experiencing improved vision within the first 24-72 hours.

